When I was first diagnosed with MS, or relapsing-remitting multiple sclerosis to be precise, I did what most doctors do when they are diagnosed with something serious – I began reading the latest research. I was distressed to discover that within ten years of diagnosis, half of those with MS are unable to work due to severe fatigue and a third have a gait disability.
Multiple sclerosis is a chronic inflammatory disease in which the immune cells attack and damage the brain and spinal cord. At first the episodes are marked by periods of worsening, (relapses) and periods of improvement (remissions). Over time, the damage accumulates, and the brain and spinal cord slowly shrink, and the level of disability steadily increases. Each patient is uniquely affected due to the specific location of the accumulating damage.
My Multiple Sclerosis story
Doctors prescribed me the newest drugs, but I continued to decline. A vegetarian for 20 years, I considered the Paleo diet – which mimics the basic diet of our pre-agricultural hunter-gatherer forebears – which claims to have the potential to treat auto-immune conditions.
According to Paleo diet advocate Loren Cordain, by not eating grains, legumes (pulses) and dairy – foods that were introduced into the human diet 10,000 years ago – patients will have fewer dietary lectins (proteins found in most plants). Cordain’s theory is that dietary lectins increase inflammation in susceptible patients. He also theorised that some patients with rheumatoid arthritis would have fewer symptoms if they consumed less lectin-containing food.
I read Cordain’s article in Mayo Clinic Proceedings, which examined the differences between Paleo and the modern Western diet and the theoretical benefits of using the palaeolithic diet to reduce the risk of cardiovascular disease. I decided the risk of adopting his dietary suggestions in an attempt to slow my decline was low, so I went back to eating meat.
Read more: Explainer: what is multiple sclerosis?
The next year my illness transitioned to secondary progressive multiple sclerosis. In this phase, no spontaneous remissions occur. Once lost, functions are gone forever. I got the recommended tilt-recline wheelchair. In an effort to slow my decline I underwent chemotherapy to deplete my immune cells and make it more difficult for them to continue their assault on my brain and spinal cord. But it didn’t work.
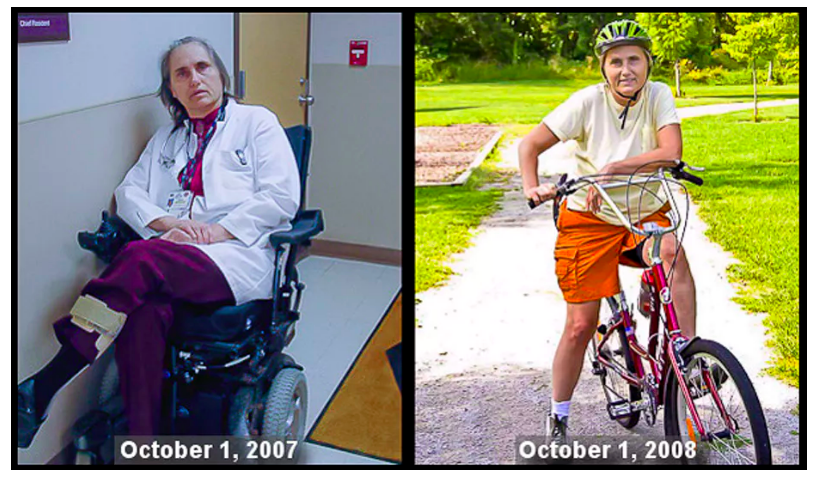
By 2007, seven years after my initial diagnosis, I was too weak to sit up in a regular chair. I was constantly exhausted and had increasingly severe bouts of trigeminal neuralgia – intense jolts of electrical face pain that were harder and harder to stop.
That summer I researched what I could do to protect my brain, focusing on vitamins and nutritional supplements to further support my mitochondria – the powerhouse for each cell. According to one theory, brain diseases may be more severe due to mitochondria that are not working well. I began taking more supplements to support my cell health, but still little changed.
So I decided to self-experiment, hoping, if I was lucky, to slow the progression of my MS. As a doctor, I certainly did not expect to walk around the hospital again making my rounds. Or go hiking or biking again. Or lead an important clinical trial testing my theories on using diet to treat multiple sclerosis–related fatigue. But that’s what happened.
My new diet Multiple Sclerosis diet
By identifying the key nutrients important to brain health, I redesigned my paleo diet. I wanted to maximise my intake of the nutrients I’d been taking in supplement form – getting them instead directly from the food I ate.
The new diet I created dramatically increased my vegetable intake: each day I consumed three platefuls of green leafy vegetables, sulphur-rich and deeply pigmented vegetables, and ate meat in moderation while eliminating gluten-containing grains, eggs, dairy and legumes. I also added fermented foods, full of good bacteria for digestive health, mineral-rich seaweed and more nutrient-dense organ meats.
ORDER HERE: https://www.lilyandloaf.com/pro-b11
Maintaining healthy gut flora helps us to digest and absorb proteins and produce B vitamins. It also helps to protect the gut wall and prevents more harmful organisms from establishing themselves.

Shutterstock
Three months after starting the diet, my fatigue was gone. The electrical face pains were gone too. I began doing my hospital rounds using a cane. After six months, I began walking without a cane. At nine months I got on my bike again for the first time in six years and biked around the block. After 12 months of this new way of feeding my cells, I biked 18 miles with my family. If I went off the diet, the electrical face pains came back within 24 hours.
Looking at the science
Paul Rothman, Iowa University’s then-chief of medicine, asked me to write a case report because recovery from progressive multiple sclerosis is rare. I worked with my treating medical team, who wrote up my case, which documented my dietary changes, supplements, neuromuscular electrical stimulation treatment and intensive physical therapy.
Rothman also asked me to write up the protocol that I had used to conduct a safety and feasibility study. My protocol included diet, stress reduction, exercise and electrical stimulation of muscles. The pilot study suggested that the complex protocol “may reduce fatigue and improve quality of life of subjects with progressive MS”.
Since then, we have conducted two more small pilot studies with favourable results showing that the dietary intervention is safe and can be sustained by over half of the people who begin the protocol. The National Multiple Sclerosis Society is funding our clinical trial to test the effect of diet on fatigue. It will complete in 2020.
Now, the idea that diet has an impact on multiple sclerosis is being considered by MS researchers, and many neurologists and patients. However, neurologists at the US National Multiple Sclerosis Society, said: “While many different dietary strategies are being promoted for people with MS, currently there is insufficient evidence to recommend any of these strategies.”
Until the results from my clinical trial are in, we won’t be able to say how effective my dietary protocol is at reducing fatigue in people with multiple sclerosis. But from my own experience, what I eat does matter.
Read more…
Three Things You Can Do To Decrease Inflammation That Causes and Advances Many Common Diseases.
Is depression a mental or physical illness? Unravelling the inflammation hypothesis
How To Do The Low Carb/Ketogenic Diet – Part 1…and Part 2: Lose Fat, Feel Better, Have Energy
Can A Vegan Or Vegetarian Do A Low Carb/Ketogenic Diet?
Terry Wahls, Clinical Professor of Internal Medicine, University of Iowa
This article is republished from The Conversation under a Creative Commons license. Read the original article.


Sending you prayers, I was diagnosed in 2010 and seemed to go down hill quickly. In six years I could no longer work and had real problems with balance and joint pain. Brain fog was really bad sometimes. I took rebif and had a lot of problems and had to quit. I have been on techfadera (not spelled right) for a few years and have several side effects. I felt lost and decided to quit my meds due to side effects. Our care provider introduced me to Ayurvedic treatment. I had a total decline of all symptoms including vision problems, numbness and others. Sometimes, i totally forget i ever had MS. I am very pleased with this treatment. I eat well, sleep well and exercise regularly. God bless all MS Warriors