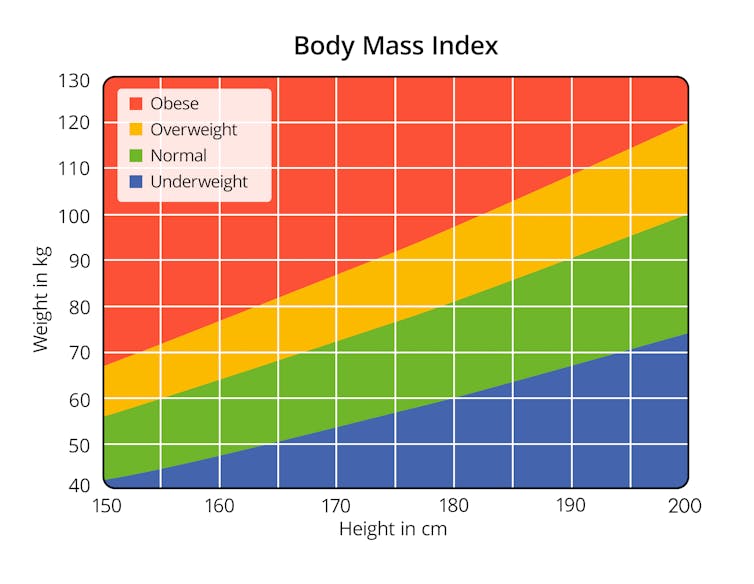
Your body mass index (BMI) indicates whether you are within a healthy weight range based on your height. Having a higher BMI – meaning more weight relative to height – can increase your risk of developing heart disease, cancer and type 2 diabetes. While BMI is partly determined by your environment and lifestyle – including your diet and how much you exercise – our genes also play a role.
Genes are inherited from our parents. When this genetic information from the egg and sperm combine, the DNA is replicated continuously – doubling the number of cells until an entire baby is formed. DNA replication is not perfect and every single base in the human genome – the single blocks of code which make up entire DNA strand – has the potential to be mutated for good or for bad. Importantly, this creates a huge amount of random genetic variation at a population level, which is like a huge natural genetic experiment. If we know that these random genetic changes are linked to small changes in BMI, we can test whether BMI influences lots of different things, including cardiovascular health – like a randomized controlled trial.
Broadly, there are two ways of identifying parts of our DNA which are linked with particular traits. Studies of patients affected by rare obesity-related disorders (candidate gene studies) or large-scale population-based genome-wide association studies (GWAS). Findings from the latter of these methods – studies that look to see whether a change at any position in our DNA is linked with a particular trait – have implicated hundreds of common genetic variants associated with BMI.
A 2015 study conducted by the Genetic Investigation of Anthropometric Traits (GIANT) consortium and published in Nature found 97 places in our DNA which influence BMI levels and which were responsible for small differences between people, regardless of how different their environment and lifestyles were. This means that, while we cannot predict an individual’s BMI with genetics, we can refer to genetics to understand if patterns materialise in populations.
Small, genetically driven changes in BMI provide an opportunity to determine whether differences in BMI between people have a role in health and disease. Genetic mutations which are randomly allocated at conception aren’t easily changed by our environment and experiences later in life. As a result, our BMI, weight and chances of developing obesity-related diseases could partly be determined before we’re even born.
Low BMI, low heart disease risk
Using this property of genetic variation, we undertook a study that was recently published in the scientific journal Circulation. Our research showed that higher BMI is likely to have an influence on measures of cardiovascular health, such as blood pressure, in more than 3,000 healthy 17-year olds from the Avon Longitudinal Study of Parents and Children (also known as the Children of the 90s).
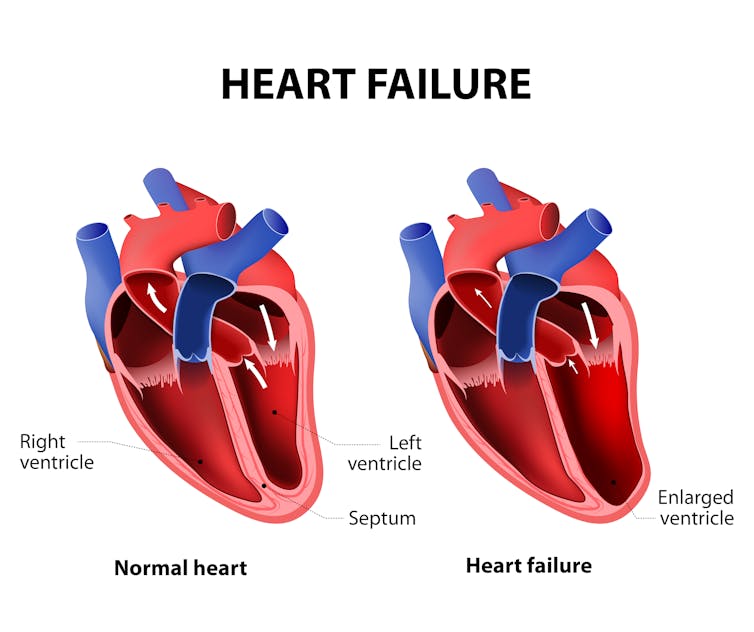
The Children of the 90s study, based in Bristol, has followed families in the UK through data collected from questionnaires, clinics and biological samples since the early 1990s. Using MRI scans from 400 21-year old Children of the 90s participants, who were recruited based on genetically driven differences in BMI, we also demonstrated that having a higher BMI is likely to lead to structural damage to heart tissue, including an enlarged left ventricle – the heart’s main pumping chamber.
Until now, studies have typically looked at the link between BMI and cardiovascular health in adults by observing patterns within populations. However, it’s difficult to conclude a relationship between the two without confusing the role that lifestyle factors play or finding how cardiovascular disease changes BMI rather than the reverse. Surveying people is also open to many sources of bias, such as recalling or reporting information incorrectly.
We wanted to isolate the property of genetic variation to improve our confidence in drawing conclusions about the relationship between BMI and cardiovascular health in a population of healthy young people.
Our results support the idea that having a healthy, normal BMI from a young age is likely to maintain a healthy cardiovascular system and help prevent heart disease later in life. Modern genetics allow us to investigate the causes of disease more quickly and cheaply than ever before, and the availability of genetic data in studies such as the Children of the 90s means we can more readily overcome limitations of traditional studies. We hope these findings lead to increased efforts to tackle the obesity epidemic at all stages of life, starting in early age.
Kaitlin Wade, Research Associate in Genetic Epidemiology, University of Bristol
This article was originally published on The Conversation. Read the original article.
![]()
