There is an ongoing lively debate among healthcare professionals about whether or not obesity is a disease. Differences between those who argue that it’s a disease and those who argue that it’s just a risk factor for conditions such as type 2 diabetes and heart disease are unlikely to be resolved any time soon. The debate, however, raises other questions, such as, what exactly is a disease and who gets to decide?
A simple definition of disease is an “illness or sickness characterised by specific signs or symptoms”. But it is interesting that some dictionaries suggest that diseases are caused by “bacteria or infections”, seemingly dismissing psychological and noncommunicable conditions as diseases, which is odd given that noncommunicable diseases, such as cardiovascular disease and cancer, make up most ill health in the world today.
Official catalogue of disease
On a global level, diseases are catalogued by international groups of experts for the World Health Organisation (WHO). This catalogue, the International Classification of Disease, is now in its tenth revision (ICD-10). Despite its name, the classification doesn’t stop at diseases but includes related health problems, which may be linked to a particular disease, or may be a symptom as part of a syndrome or even a consequence of a medical procedure. For example, even dehydration appears in ICD-10, where it is also called “volume depletion”. So perhaps there is not even agreement on what is meant by disease. And what is classified as disease is essentially down to expert consensus.
While the WHO doesn’t seem to have a clear definition of disease, it does at least have a definition of health. It is defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”.
The definition of health appears to be broad and inclusive, but defining disease appears to be more challenging than defining its opposite. Few people would disagree that measles, say, is a disease. But what happens when society decides to classify a certain human behaviour or characteristic, which some groups happen to find disturbing, as a disease.
Sin as a source of disease
Examples of classifying characteristics as diseases can be seen throughout human history. Many of these might be grounded in traditional beliefs and views of health, disease and their links to sin.
The development of psychology as a science potentially led some perceived “sins” to be translated into mental health disorders. Perhaps the best example of this is homosexuality. Homosexuality was classified as a mental disorder by the American Psychiatric Association (APA) in 1968. This was later challenged by a vote among APA members in 1973, where a majority of 58% chose to remove it from the diagnostic manual. Homosexuality was not fully removed from the diagnostic manual for another decade and is now considered to be a normal characteristic within the diversity of human nature.

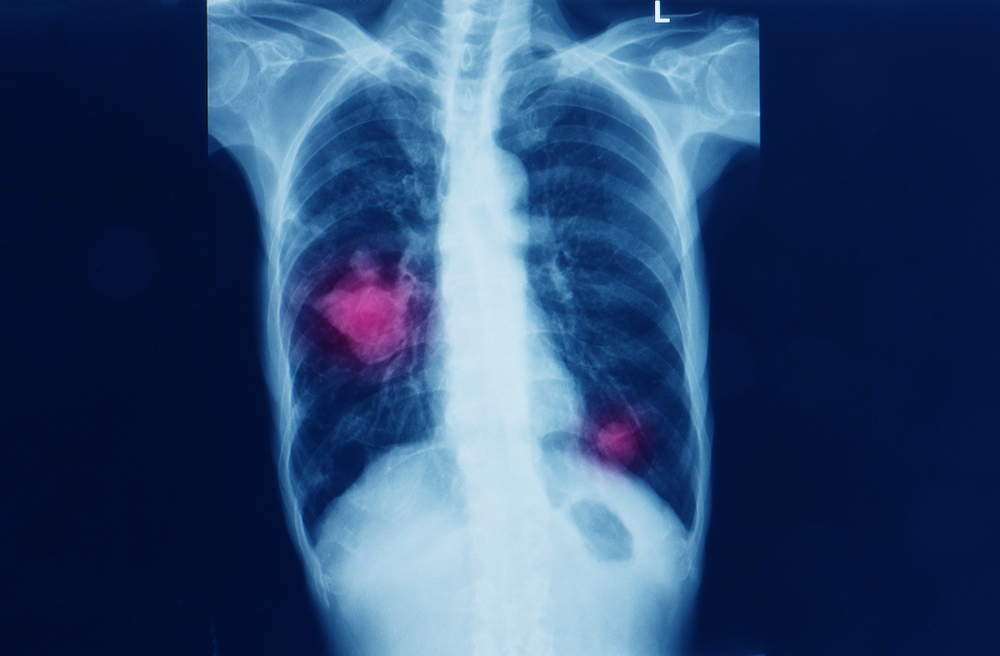
lazyllama/Shutterstock
This disturbing episode raises further questions: on what basis and in whose interests are diseases classified?
In 2013, researchers at Bond University in Australia looked at who gets to classify diseases. They found that common diseases often had their definitions widened by expert groups, without considering the potential risks or challenges of increasing the number of people living with disease. They also noted that experts who widened definitions of diseases often have conflicts of interests in the form of funding from pharmaceutical companies.
On the spectrum
Sometimes, risk factors for a disease – such as high blood pressure – eventually get defined as a disease in their own right. And once these risk factors are reclassified as a disease, their targets or ranges tend to shift over time, increasing the number of people who have the disease. For example, high blood pressure used to be anything over 140/90. But in 2017, the US changed the threshold to 120/80.
Distinguishing a disease from a risk factor is not easy, especially when it comes to chronic diseases, which tend to be a spectrum from health to illness. Blood glucose (sugar) is a clear example as levels move from healthy through pre-diabetes into type 2 diabetes. So spotting where health finishes and disease begins is difficult, to the point that the WHO and International Diabetes Federation suggest there is no such thing as a normal level of blood glucose.
Nevertheless, the definition of gestational diabetes (diabetes in pregnancy) changed in 2014, when the blood glucose threshold was lowered. The change increased the incidence of gestational diabetes by 74% with no improvement in short-term outcomes, such as the mother needing a caesarean section, according to one Australian study.
Many clinicians are critical of this trend, calling it over-medicalisation.
Normal ageing or disease?
Sometimes, conditions previously thought of as being a natural part of getting older have become diseases. For example, osteoporosis was considered a normal part of ageing until 1994 when the WHO officially recognised it as a disease. Given osteoporosis’s link with an increased risk of fractures and the devastating impact broken bones can have on the elderly, this seems like a change in definition that is justified.
Other physiological changes that occur in older age, such as a fall in testosterone levels in men, may not benefit from disease status. But that hasn’t stopped some healthcare experts trying to create a new condition called “the andropause”. So far, though, resistance to recognising this change as a disease has been strong.
All of the above goes to show that deciding what is or isn’t a disease is not easy, but hopefully you’ll be better equipped to ask some critical questions such as, who benefits from this new definition? And do they have my best interests at heart? The answer to the latter question is usually yes – but not always.
Duane Mellor, Senior Teaching Fellow, Aston Medical School, Aston University and Shahid Merali, Clinical Senior Lecturer: Lead for Primary Care Education, Aston University
This article is republished from The Conversation under a Creative Commons license. Read the original article.