Updated blood pressure guidelines from the American Heart Association mean that many more Americans, notably older people, are now diagnosed with high blood pressure, or hypertension. This may sound like bad news, but the new guidelines highlight some important lessons we cardiologists and heart health researchers have learned from the latest blood pressure studies. Specifically, we have learned that damage from high blood pressure starts at much lower blood pressures than previously thought and that it is more important than ever to start paying attention to your blood pressure before it starts causing problems.
High blood pressure accounts for more heart disease and stroke deaths than all other preventable causes, except smoking.
As president of the AHA and a cardiologist, I completely support the latest guidelines. I know they will save lives, especially when blood pressure is accurately checked and when people make therapeutic lifestyle choices to lower their blood pressure.
How high blood pressure damages
High blood pressure, which occurs when the force of blood pushing against blood vessel walls is too high, is similar to turning up the water in a garden hose – pressure in the hose increases as more water is blasted through it. The added pressure causes the heart to work too hard and blood vessels to function less effectively. Over time, the stress damages the tissues within blood vessels, which can further damage the heart and circulatory system.
The AHA, the American College of Cardiology and nine other health professional organizations reviewed more than 900 studies as part of a rigorous review and approval process to develop this first update since 2003 to comprehensive U.S. high blood pressure guidelines.
Here’s what’s new:
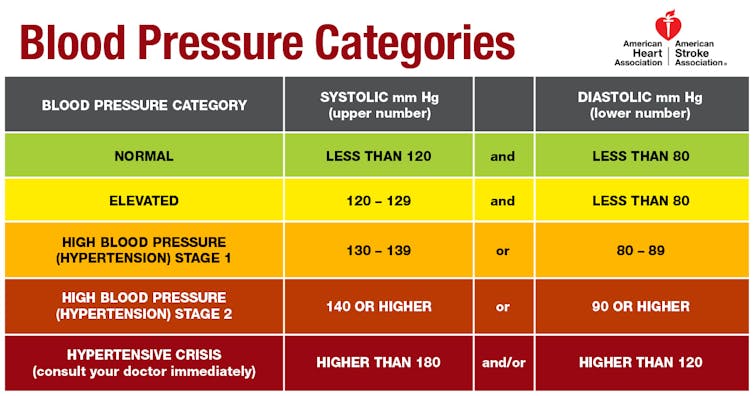
- High blood pressure, previously defined as 140/90 mm Hg or higher, is now defined as 130/80 mm Hg or higher. This change reflects the latest research that shows health problems can occur at those lower levels. Risk for heart attack, stroke and other consequences begins anywhere above 120 mm Hg (for systolic blood pressure, the top number in a reading), and risk doubles at 130 mm Hg compared to levels below 120.
- Blood pressure in adults will be categorized as normal, elevated, stage 1 hypertension or stage 2 hypertension. The category “prehypertension” is no longer used; it previously referred to blood pressures with a top number (systolic) between 120-139 mm Hg or a bottom number (diastolic) between 80-89 mm Hg. People with those readings are now categorized as having either Elevated or Stage I hypertension.
- Determination of eligibility for blood pressure-lowering medication treatment is no longer based solely on blood pressure level. It now also considers a patient’s risk of heart disease or stroke over the next 10 years, based on a risk calculator. For people with blood pressure higher than 140/90 mm Hg, medication is recommended regardless of risk level.
Putting the guidelines to work
Hypertension is known as the “silent killer” because often there are no obvious symptoms. The only way to know whether you have it is by having your blood pressure measured. Accurate blood pressure measurement is critical to a correct diagnosis.
The guidelines emphasize use of proper technique to measure blood pressure, whether taken by a health care professional in the clinic or by the patient using a home blood pressure monitoring device. Blood pressure levels should be based on an average of two to three readings on at least two different occasions.
A number of common errors can inflate a reading. These include having a full bladder, slouching with unsupported back or feet, sitting with crossed legs, or talking while being measured; using a cuff that is too small or wrapping the cuff over clothing; and not supporting the arm being measured on a chair or counter to keep it level with the heart.
An accurate reading is critical to a correct diagnosis, faster treatment and the most appropriate care.
The lower threshold for a diagnosis of high blood pressure increases the percentage of U.S. adults (ages 20 and older) who have the condition, from approximately 1 in 3 to nearly half (46 percent).
Even with the new threshold, the percentage of U.S. adults for whom medication is recommended (along with lifestyle management) will increase only slightly. Most of the people who are newly diagnosed with high blood pressure will be advised to make lifestyle changes to shift their blood pressure into a healthy zone.
The promise of healthy lifestyle changes

Damage to blood vessels begins soon after blood pressure is elevated. Early intervention can help prevent problems, slow damage that has already started and lower the risk for a heart disease or stroke. Lifestyle changes should be on the front lines of efforts to tackle the high blood pressure epidemic.
Here are some of the best proven nondrug approaches to prevent and treat high blood pressure:
- Lose weight. For each kilogram lost, systolic blood pressure is expected to fall by about 1 mm Hg.
- Eat better. Choose a dietary pattern rich in fruits vegetables, whole grains, and low-fat dairy products, reduced in saturated and total fat, lower in salt (aim to cut current intake by 1,000 mg/day sodium), and rich in potassium (aim for 3,500-5,000 mg/day, focusing on potassium-rich foods such as bananas, potatoes, avocados and dark leafy vegetables).
- Move more. Get 90-150 minutes per week of both aerobic physical activity and resistance training.
- Moderate alcohol intake. Limit to one drink or fewer per day for women and two drinks or fewer per day for men.
Personal responsibility for one’s health behaviors is important, but a number of other complex, interrelated aspects of the physical, social and policy environments influence these behaviors.
Public health practices and policies leading to changes in systems and environments support individuals’ efforts to make healthy lifestyle choices. For example, well-maintained sidewalks, bike lanes and parks support physically active lifestyles, and healthier food options in corner stores, vending machines and other public places promotes better eating habits. Community-based efforts can shift social norms and help transform the environments where behaviors occur to make healthier choices easier – more accessible, affordable, and attractive – for everyone.
John Warner, Executive Vice President, Health Affairs, UT Southwestern Medical Center
This article was originally published on The Conversation. Read the original article.
![]()

